Eczema, Atopic Dermatitis & Topical Steroid Withdrawal Case Studies & Treatment (Part 2)
This article is part two in a two-part series. Click here for Part 1.
Case Study: Topic Steroid Withdrawal and Chinese Herbal Medicine Treatment
Case Study Intro
As discussed in Part 1 of this two-part series, treatment of skin disease first involves getting a sense of what condition is presenting, in what pattern(s) has it presented over time, and finally what are the unique features of the current presentation. With this information, an herbal formula is constructed to address the diagnosed disease in its current manifestion to help bring the individual’s health back into a more harmonious state.
What follows is the case of M.J., an 18 year old male who sought treatment for "eczema" and "topical steroid withdrawal (TSW)" in October, 2021.
Case History
M.J. was accompanied by his father during his initial visit on October 15, 2021. M.J. was seen twice per month until the first week of January 2022, returning every 4 to 6 weeks until the first week of May 2022, after which treatment ended. The patient was contacted via e-mail in July, 2023 before this article was written to be certain there were no unreported flare ups since treatment was concluded.

M.J. was treated primarily with Chinese Herbal Medicine in granular extract form. After his skin had improved significantly, a moisturizing and anti-inflammatory Chinese herbal lotion was introduced for use mainly on his body. The patient also received red light therapy at some visits.
History of Disease and Treatments Prior to TCM
M.J. reported suffering from atopic dermatitis since he was 3 or 4 years old, with lesions that were often in the knee flexures (behind the knee), on his calves, his forearms and elbow flexures, and under his arms in the axilla. He reported that his skin was "rough and dry, kind of like sandpaper" and that as a child he hardly ever experienced fluid discharge. However, M.J. reported that as he got older, he could more easily scratch until fluid was produced, and said that both OTC and prescription topical steroids were his main treatment up until he was about 16. Reportedly, the eczema progressively worsened as he got older. Suspicious that topical steroids were actually leading to a decline in his skin or at least were not helping, M.J. reported stopping topical steroids, after which he said that stopping the steroid led to a significant flare up of his skin.
M.J.'s first major skin flare occurred approx 1.5 to 2 years prior to being seeing at my clinic. M.J. developed dark, burning, weepy lesions all over his chest and back. Suffering significantly, M.J. was treated with oral prednisone and was put on topical steroids once again.
Attempted Treatment Through Diet
Following the initial flare up, M.J. made significant efforts to live a healthier life. The patient is approx 6' 1" and reported that he previously weighed "280 lbs", "ate a lot of hot wings" , and was chronically "constipated". At the first visit, the patient weighed only 189 lbs. The patient reports that he stopped eating fast food, started eating a lot of vegetables, ate a lot of wild salmon, and started exercising regularly as long as his skin did not prevent him from doing so. At that time, which was a few months before his initial visit with my clinic, he also stopped using topical steroids. I do believe the lifestyle and dietary changes allowed for faster improvements once he started taking Chinese herbs.
The Beginnings of the Current Flare Up
As per M.J., he tried to reduce topical steroid use again during Spring, 2021, resulting in a significant outbreak by Summer, 2021. The patient reported he again developed a deep red burning rash on his chest and back and progressively worse lesions on his neck and face. M.J. initially began to suffer a deeply erythematous maculopapular rash (one large dark red elevated lesion) that covered the anterior neck. With time, the skin on the front of M.J.'s neck eventually eroded and became a large open wound with significant fluid discharge emitting from it.
At the start of this outbreak, the patient began developing red papules on his cheeks, almost acne like. These lesions continued to progress until they covered his whole face, with white and slightly yellowish crusting scales from mild fluid discharge.

Attempted Therapy with No Moisture Treatment (NMT)
NMT is a therapy that restricts moisture and fluid intake, and M.J. stated that he stopped applying topical moisturizers since the beginning of this flare up and also limited the number of showers he took, along with his intake of fluid, which he said seemed to help, but was not sufficient to resolve the lesions.
As M.J. was progressively getting worse, he visited his medical team and was again prescribed oral prednisone in August, 2021. Reportedly, the second round of prednisone did not bring a full recovery like the first round did and soon after, he noticed that his skin was again starting to worsen with facial redness, scaling, and peeling. M.J. stated that he did not want to do yet another round of oral steroids or to restart topical steroids. The patient continued with the no moisture treatment and pursued other options, which eventually led him to my Chinese Medicine clinic on October 15, 2021.
Further Information Reported on Inquiry
Heat and Sleep: At the initial visit the patient stated that he ran warm at all times and could sweat very easily. M.J. reported discomfort with worsening symptoms after exposure to strong sunlight or any type of heat. M.J. also stated that he felt even warmer at night and reported near total insomnia during evening hours since the flare up started. M.J. states that he was unable to sleep until about 5 A.M or 6 A.M every day, being sleepless during the night. The patient also reported itching that intensified at night , adding to his sleeplessness and discomfort.
Thirst: Despite significant heat signs, M.J. reported no significant thirst.
Bowels: The patient reported regular bowel movements having solved his constipation issues by changing his diet over the previous two years.
Pulse: Notably weak for an 18 year old male. The pulse was also somewhat thin. HR: 68 BPM

Tongue: Thin white coat, pinkish red body
Medications: None
Description of Presenting Lesions: In the practice of TCM dermatology, the diagnostic skill of observation is extremely important. Just by looking at the patient and the nature of the lesions, it was clear that he was most likely suffering severe temperature dysregulation, likely having insomnia, and definitely itching amongst other things. These observances about the patient's health would, in part, lead to a plan of care in order to bring him into better harmony and health.
On his face, the patient presented with a mask-like appearance consisting mostly of semi-adherent white exfoliative scales. The scaling was mixed with some crusting that had a mild, off-white coloring. No significant yellow crusting was present. There were bloody excoriation marks in some areas of the face as well. The nose was covered in scaling. The lips were peeling. The skin on the face was generally dry.
There was a mild erythema (redness) on the cheeks and around the eyes however it was not immediately evident as the crusts and scaling made it difficult to see. The crusts and scaling stopped at the beard area.
The neck presented with macular erythema that was much easier to see than on the face. The patient reported that the eroded skin on his neck had healed with the oral prednisone two months prior. However, at that moment, the anterior neck presented with a large brightly erythematous macule with slightly laminate (glassy) skin indicating increasing erythema and activity.
The patient's chest and back appeared checkered as there was a mixture of active slightly hyperpigmented papules and plaques with inactive post-inflammatory pigmented macules. There were also many excoriated papules on the chest and back. The skin on the upper chest and back that was unaffected by papules presented with a mild erythema. The skin unaffected by papules or pigmentation on the lower abdomen and lower back did not present with erythema. Some maculopapular lesions on the chest and back blanched upon pressing them, others did not blanche.
The legs presented with dry skin, scattered excoriated papules, heavily hyperpigmented active papules and hyperpigmented, but fading, post-inflammatory macules. Behind the knees there were healing, but still active, small plaques that were hyperpigmented, fairly thin, but still not flat. There were a few excoriation marks behind the knees.
The upper arms and shoulders presented similarly to the chest and back with a mixture of active erythematous papules, plaques, and hyperpigmented macules. The elbow flexures and lower arms presented without many papules, macules, or post-inflammatory hyperpigmentation. However, the elbow flexures had a very mild and subtle erythema, not untypical of eczema.
Differential Diagnosis
TCM Diagnosis: Wind Of The Four Crooks complicated by topical steroid withdrawal syndrome.
The patient's history clearly indicates that he suffered from atopic dermatitis throughout his life, with a long history of lesions behind his knees and elbow creases that spread to more regions as he got older. As far as considering the progression and flare ups due to topical steroid withdrawal (TSW), of course the history of topical corticosteroid use is one factor, while burning lesions is another. In addition, while eczema can and will present on the face, TSW has almost become synonymous with the presentation of either extreme erythema of the face, neck, and/or arms and/or large areas of red peeling skin including on the entire face. In terms of the dermatological diagnosis criteria, it is always worthwhile to factor this in so that we become sharper in distinguishing the different lesions and distinguish the sometimes minute differences between skin diseases.
Both seborrheic dermatitis and psoriasis can present on the face and also progress into more severe erythrodermic presentations just as atopic dermatitis (AD). All three conditions are itchy and all three can affect the face. With seborrheic dermatitis, we would have expected a long history of either dandruff, generalized scalp inflammation, lesions around the eyebrows, side of the nose, or on the sternum that for various reasons, including improper treatment, could lead to a severe outbreak on the face that spreads to the body as well. M.J., however, started as a child with lesions on his body that did not spread to the face until stopping topical steroids. Therefore, this diagnosis was ruled out.
With psoriasis, we would expect a history of psoriatic types of lesions which differ from M.J.'s presentation. The papules in psoriasis are typically thicker with well defined circumscribed edges. With M.J., there were papules on the body without scales while on the face there were scales mixed with crusting, but without underlying papules. Not only did M.J. never have a history of these thick psoriatic type lesions, but psoriasis on the scalp is significantly more common than it is on the face (Dopytalska, 2018; Egeberg, 2020). Though it does occur, psoriasis on the face only occurs in a minority of cases, and usually does not cover the whole face. However, it is plausible that a patient with erythrodermic psoriasis could present with exfoliation of the face similar to M.J. Simply looking at photos of the face, it may be impossible to tell the underlying disease leading to the erythema. However, taking a simple history and inquiring about the history of the disease and its lesions, it should be easy to differentiate the two diseases. M.J. also reported a previous history of classical eczematous lesions.
In particular, the history of lesions in the four flexures, or the “four crooks”, amongst other areas, clearly indicated that the patient suffered from Wind of The Four Crooks (atopic dermatitis) while the repeated intense flare ups that started after ceasing topical corticosteroids and spread to previously unaffected regions indicated a significant complication of topical steroid withdrawal syndrome.
TCM Pattern Diagnosis
M.J.'s history of recalcitrant atopic dermatitis that spread rapidly and widely over the body with burning lesions, the experience of significant heat with insomnia, intolerance to the heat and sun, and exfoliating skin are symptoms of Fire Toxin with Heat in the Blood & Ying Level.
When discussing exuberant heat and the Four Levels of Warm Disease differentiation, "the presence or absence of thirst is an indication of whether heat remains in the Qi Level or has moved to the nutritive level" (Scheid et al., 2009). Heat in the Qi level depletes Stomach fluids leading to thirst. Once the heat progresses further to the Ying level, thirst stops. Despite intense heat all day and especially at night, M.J. reported no thirst, indicating heat in the Ying level.
In reviewing the lesions, the anterior neck presented with bright red/ pink macular erythema with ill defined edges that seemed to be spreading, corresponding with an indication of Fire. Some maculopapular lesions on the chest blanched with pressure, indicating Heat in the Qi or Blood Level, while others did not blanch, indicating Extreme Heat (Al-Khafaji, 2016). Other paler lesions indicate just heat without spreading.
While Dampness and Heat are etiological factors in all cases of atopic dermatitis, some cases develop presentations more solely driven by these factors. We know that M.J. had a long history of lesions under his arms in the axillary cavity and fluid discharge with large eroded lesions on his neck as he got older. These are all symptoms of a Damp Heat pattern. The dryness the patient presents with can also be considered to be due to Damp Heat as the dampness obstructs the flow of Qi, Blood and nourishment to the skin, while the heat dries out the skin. It would be inappropriate to treat the dryness directly with warm tonics while there is so much activity and active heat signs. Addressing dryness as a pattern itself will take place later in treatment.
All signs and symptoms considered, the clinical relevance of the spreading Heat signs are taken more seriously, especially given the history and trajectory of the disease. The pattern is thus considered to be Fire Toxin with Heat In The Blood & Ying Level complicated by Damp Heat.
Treatment Principles
Similar to my Lichen Planus case study published with Mayway Herbs, the primary CM Treatment Principles employed in this case (and most skin diseases I treat) are to:
- Drain Pathogens (Acute Phase)
- Harmonize (Middle Phase)
- Tonify (Consolidation/Prevention Phase)
Initially draining involves draining Heat and resolving Toxin (via stools but not in a purgative fashion); venting Heat and Toxin from the Ying level to the Qi level; venting Heat and Toxin to the surface; clearing the Qi Level, drying Dampness; and draining Dampnes and Heat via the urine.
Phase 1: Drain Pathogens
The initial formula employed the following Treatment Principles and herbs:
The initial and main formula is loosely based on the principles of Wu Ju Tong's Qing Ying Tang and a formula template taught by Mazin Al-Khafaji for Toxic Heat in The Qi, Ying, and Blood level pattern of atopic dermatitis. The formulas were modified significantly to fit the patient's presentation, which the author feels presented with more constitutional Dampness than the original formulas were intended for.
- Huang bai and Huang lian: Bitter and cold herbs Huang bai and Huang lian were used to clear Heat, drain Fire, resolve Toxin, and dry Dampness.
- Xuan shen and Bai mao gen: Salty and cold Xuan shen and Sweet and Cold Bai mao gen both cool the Ying and Blood Level while supporting Yin and fluids. Typically, large doses of Sheng di huang would be used as the main herb for those functions. However, due to the patient's history of a more extreme Damp presentation, I preferred to avoid Sheng di huang initially, despite it being excellent at cooling the Blood and nourishing Yin and Fluids. However, I did use a moderate amount (equivalent to 7 - 9g of raw herb) of warm and sweet Shu di huang to nourish Yin and treat deficiency Heat. The prolonged nature of the patient’s eczema over many years and the two recent severe flare ups with extreme heat symptoms and the thin and weak pulse lead me to believe there was some Yin deficiency. The moistening aspect of these three herbs would also help buffer the necessary dryness of the other herbs used in the formula.
- Zi cao: Acrid, salty, and cold Zi cao along with acrid and cold Mu dan pi cool the Ying and Blood and prevent stagnation.
- Ye ju hua: Light, acrid, cold Ye ju hua is used to vent Heat and Toxin from the surface. Ye ju hua has an affinity for the face and is useful in Damp Heat presentations as well. Therefore it was used to replace light, acrid, and cold Jin yin hua and Lian qiao used in Qing Ying Tang, where they help to vent heat from the nutritive to the Qi level and to circulate Qi in general to prevent stagnation (Guo, 2008).
- Zhi mu: Cold and acrid Shi gao was used with cold and sweet Zhi mu to help venting to the Qi level. Zhi mu also helps nourish Yin and fluids and to moderate the other drying but necessary herbs.
- Ban lan gen: Bitter and cold Ban lan gen was used in moderately large dosage to resolve Toxin and drain Heat from the blood. Whereas Ye ju hua works on the more superficial levels, Ban lan gen works on the Blood level.
- Dong gua pi and Di fi zi: Bland, sweet, and cold Dong gua pi was used to eliminate dampness and heat via the urine. Dong Gua pi excels at treating damp eroded skin. Bitter and cold Di fu zi also promotes urination to drain dampness while its bitterness drains fire. Di fu zi is known to stop itching as well. In Qing Ying Tang, light, acrid, cold Dan zhu ye is used to vent heat from the Qi level and via urine. Due to differences in the patient's constitutional presentation and concerns of dampness, Dong gua pi and Di fu zi were used instead.
- Bai ji li: Light, acrid, warm/neutral Bai ji li scatters Qi from the surface to reduce itch. Bai ji li is better for itching in the upper body, while Di fu zi has a stronger effect on itching in the lower body.
The herbs were prescribed for 14 days in the form of granular extracts; 36 grams in total per day. The patient was instructed to split the daily dosage into 2 or 3 separate doses, dissolving the granules in hot water. Exact dosages are not provided here, as this formula is not presented with the intention of it being appropriate for every Topical Steroid Withdrawal patient.
Discussion Of Results
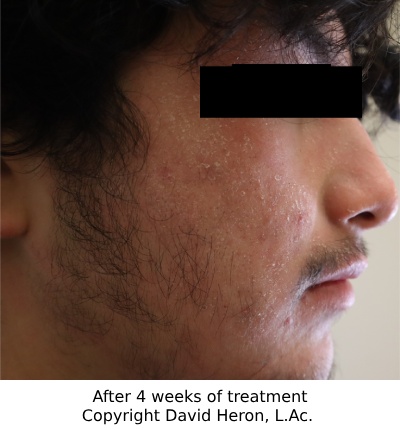
Visit Two, Two Weeks Later

At the first follow up visit, after two weeks as we walked back to the photo room, M.J.'s father seemed upbeat and stated that he thought the "scales on the face are getting thinner". It was true, the scales on the face had reduced slightly, by approx 30%. As the scales reduced, background erythema was more prominent. The patient reported reduced itching of his face, although also reported some slight fissuring around the lips. He also reported ongoing itch on his chest and back. Upon examination, some of the active lesions on the back from the previous visit were now more hyperpigmented and becoming thinner or healed. There was one small area of crusting on the back, and the patient stated that he repeatedly scratched that spot and it eventually began to discharge a minute amount of fluid.
Visually the greatest improvement over two weeks was in the left knee flexure where the previous maculopapular rash had mostly cleared. However, I believe the most significant improvement was that the patient reported he fell asleep "at a normal hour" a handful of times over the last two weeks. The patient reported that he was still running warm, and he denied thirst.
The previous formula was modified. Huang bai and Dong gua pi were reduced so as not to be as drying due to the lip fissures and Bai shao was added to address them. Zi cao was replaced by Hu zhang, focusing on greater ability to resolve Toxins. Lian qiao was added for the same reason. Di fu zi was removed due to its drying nature and because the itch was more severe in the upper body. Bai ji li was also replaced as the effect was unclear. Xi xian cao and Bai xian pi were added to expel Wind Dampness and stop itch.
Visit Three, One Month Since Starting Treatment
After one month taking the herbal formula daily, M.J. reported and demonstrated significant improvements in every area. He reported almost regular sleep hours and ability to sleep during the night starting at 10 or 11 P.M. The patient reported a marked reduction in heat but still felt warmer at night.
Scaling and erythema of the face had reduced significantly, were progressing on pace, but were yet to resolve fully.
Itch had reduced on the upper body and the patient now reported that itch on the lower body bothered him more.
The dry fissures around the mouth had resolved completely meaning the Bai shao and other modifications worked.
The lesions on the back were healing and a very large post inflammatory macule was developing on the entire center of the patient's back.
A few acne-like papules and pustules were developing on the patient's back and face. The patient reported they were present previously, but disappeared during the large eczema/TSW flare ups.
The previous formula was modified again. Bai xian pi was removed and Di fu zi was added due to lower leg itch. Lian qiao was replaced by Bai hua she she cao.
Visit Four, 3 Weeks Following the Previous Visit
The patient presented with significant improvement. Lesions were now roughly 90% clear since starting herbal medicine 7 weeks prior. The patient's face was mostly clear, but he reported some scaling around the eyebrows and hair loss from the area and the scalp. No lesions were seen on the scalp, but there was dandruff.
Active lesions on the back had cleared. The macule on the neck had been completely resolved. There was significant post inflammatory hyperpigmentation, with a very mild diffuse rash happening on top in some areas of the back.
The previous formula was modified, severely reducing the dosage of the dry bitter herbs. Xi xian cao was removed and Wei ling xian was added along with Bai ji li to scatter Wind from the surface and treat the scaling around the eyebrows.
Visit Five, Just Over 2 Months Since Starting Treatment
Phase 2: Harmonize
By the fifth visit on 12/18/2022, the lesions were approximately 95 - 98% clear on the face. Scaling around the eyebrows had improved but remained slightly around the left eyebrow. The patient's back continued to present with a diffuse mild rash with small scattered papules over previously healed post inflammatory hyperpigmented macules. The patient reported near normal heat and a resolution to his insomnia.
The formula was now modified as the patient had improved significantly and there were no signs of exuberant heat or skin activity. Huang lian and Huang bai were removed from the formula. Xuan shen was reduced as the focus was no longer to clear Heat from the Blood. The dosages of Shu di huang and Bai shao were increased as the primary focus of the formula was now to nourish Blood and Yin. Dan shen was added to replace Mu dan pi, as Dan shen helped to nourish and move the Blood while also resolving post inflammatory hyperpigmentation. Di fu zi, Bai ji li, and Wei ling xian were removed. Jin yin hua and Lian qiao were added to continue to clear toxicity while starting to tonify deficiency and also to address some developing acne lesions. The dosage of the formula was reduced to 32g per day.

Visit Six, 3 Months Since Starting Treatment
This was the first visit where the patient reported some non-compliance with the regimen, noting he failed to take the herbs regularly over the Christmas and New Year's Holidays. The patient had maintained all previous progress, however. He did however, develop some angular cheilitis, which is a dermatitis or irritation of the skin in the corners of the mouth. On inquiry, the patient reported eating more sweet baked goods than usual over the holidays. While angular cheilitis has many causes, it can often be due to an over growth of candida albicans. This is common in eczematic patients and often seen in clinic regularly during the holiday season due to increased sugar intake.
The formula continued to be modified to move further towards tonification. A small dose of Sheng di huang was added, to assist Shu di huang in addressing dryness. Huang qi was added to tonify Qi and help the other tonic herbs to function better. Jin yin hua and Lian qiao were removed and Ji xue cao was added due to some mild acne like papules which were not progressing but improving slowly. Yi yi ren was added and the dosage of Bai hua she she cao was increased to address the acne formation. A small dosage of Huang lian was added to address the angular cheilitis.
Visit Seven, Four Months Since Starting Treatment
The patient reports ongoing and sustained significant improvement, approx 95%+. M.J. had run out of herbs as he needed to push his appointment back and could not come in until two weeks later than expected. The patient stated the flaking of the left eyebrow was not always present, but still occurred. The patient's back was free from active eczema lesions and was covered in a large pale and fading hyperpigmented macule. The color of the macule was not only fading, but had become more uniform across the back.
The patient denied exuberant heat, but did report that he had started to feel a little warmer at night. Therefore, the formula was changed despite progress to address the increase in heat before any chance of outbreak developed. As there had been no signs of extreme dampness in quite some time, Sheng di huang was now used.
The formula was to clear Blood Heat with Wind. The Wind here referred more to the scaling of the left eyelid. However, it could have applied to itch, but itch was almost absent, only occurring immediately after showering. The formula construction was more similar to ones used for Roving Face Wind (seborrheic dermatitis) as the flaking eyebrow was the only real eczematic activity of the skin and previous formulas had failed to fully address it.
The formula was 32g per day, split in two doses in hot water and consisted of: Sheng di huang, Shu di huang, Bai mao gen, Xuan shen, Shi gao, Zhi mu, Mu dan pi, Dan shen, Wei ling xian, Bai ji li, Niu bang zi, and a small dosage of Huang bai.
Visit Eight, Almost 5 Months Into Treatment
Phase 3: Light Tonification
The patient presents 99% clear of eczema. The patient reported that the left eyebrow had settled down and his face was now clear of eczema. There were still some scattered post-inflammatory lesions on his body, but they had faded significantly and appeared to be improving. He still had minor acne on his face and back, but not as serious as prior to his eczema flare ups. The patient reported that he had not been washing his face and was encouraged to begin doing that again with a gentle baby soap as there was no longer any concern of irritating his face.
The patient was given a similar formula and was seen twice more, each time reducing the dosage of the herbs. The ratio of Yin, Blood, and Fluid tonics increased each time the total dosage of herbs reduced. Light tonification was provided to consolidate the effects. Warmer herbs like Huang Qi and Dang Gui were not used as the patient still seemed to have a slight propensity towards heat as he reported slight warmth at night at visit seven. At future visits, the patient reported occasional very mild eczematous activity, such as a few small papules would present on his arm or face and resolve in a day or two time, but eventually stopped. The patient was last seen in May 2022.
My last communication with the patient was in July 2023, over a year since he was last seen and over a year and half since the last major flare up had resolved with treatment. M.J. reported no eczema aside from minor occasional skin irritation behind the knees, etc. that resolves on its own.
Closing Thoughts
How many people out there, suffering like M.J., would benefit from Chinese Medicine? Sheehan et al (1992) published in the Lancet that "we have shown that Traditional Chinese herbal therapy affords substantial clinical benefits in patients whose atopic dermatitis has been unresponsive to conventional therapy". However, just as the many published warnings about the existence of Topical Steroid Withdrawal (TSW) secondary to improper topical corticosteroid use went mostly on deaf ears, the same seems to have been true with published evidence supporting Chinese Herbal Medicine for the treatment of atopic dermatitis.
Chinese Medicine practitioners have been treating TSW for at least 40 years and have been treating erythema, oozing, scaling, peeling and all the various symptoms associated with TSW for thousands of years. Uzun et al (2021) published a great case study of a 7 year old boy suffering from TSW that was treated with Chinese Herbal Medicine. This is not an isolated achievement. Many patients suffering from TSW in the recent past, even before a name was agreed upon to the phenomena, eventually sought help outside of conventional medicine and some Chinese Medicine practitioners have long familiarity with TSW.
It is important to examine the patient’s improvements, and also to observe their behaviors. M.J. did not stop treatment after 2 weeks because he still felt warm or because there was still itch. Nor did he stop because the herbs tasted badly, which the author is 100% certain they did. Rather, at two weeks, he was pleased because he saw some signs, even if minor, of improvement. Together, we reviewed his symptoms objectively, admitted improvement where it was, detailed what still needed improvement, adjusted from there, and continued on. His father and family also played an important role in being supportive. Some patients will need to continue treatment longer than M.J. but that's okay. Atopic dermatitis can be managed wonderfully and TSW can be overcome, so please do not fall prey to a negative and bleak outlook. But rather, stay the course with your patient as they progress with their treatment.
For patients seeking a Chinese Medicine dermatologist, or for practitioner training options please visit: tcmdermatology.org.
References
- Bantz, S. K., Zhu, Z., & Zheng, T. (2014). The Atopic March: Progression from Atopic Dermatitis to Allergic Rhinitis and Asthma. Journal of clinical & cellular immunology, 5(2), 202. https://doi.org/10.4172/2155-9899.1000202
- Barta, K., Fonacier, L. S., Hart, M., Lio, P., Tullos, K., Sheary, B., & Winders, T. A. (2023). Corticosteroid exposure and cumulative effects in patients with eczema: Results from a patient survey. Annals of Allergy, Asthma & Immunology, 130(1), 93-99.e10. https://doi.org/10.1016/j.anai.2022.09.031
- Bowe, S., Masterson, S., Murray, G., & Haugh, I. (2022). Topical steroid withdrawal through the lens of social media. Clinical and Experimental Dermatology, 47(8), 1554–1557. https://doi.org/10.1111/ced.15194
- Dopytalska, K., Sobolewski, P., Błaszczak, A., Szymańska, E., & Walecka, I. (2018). Psoriasis in special localizations. Reumatologia, 56(6), 392–398. https://doi.org/10.5114/reum.2018.80718
- Egeberg, A., See, K., Garrelts, A., & Burge, R. (2020). Epidemiology of psoriasis in hard-to-treat body locations: data from the Danish skin cohort. BMC dermatology, 20(1), 3. https://doi.org/10.1186/s12895-020-00099-7
- Ference, J. D., & Last, A. R. (2009). Choosing Topical Steroids. American Family Physician, 79(2), 135-140. Retrieved from https://www.aafp.org/pubs/afp/issues/2009/0115/p135.html
- Gabros, S., Nessel, T. A., & Zito, P. M. (2023). Topical Corticosteroids. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK532940/
- Johansson, S. G., Bieber, T., Dahl, R., Friedmann, P. S., Lanier, B. Q., Lockey, R. F., Motala, C., Ortega Martell, J. A., Platts-Mills, T. A., Ring, J., Thien, F., Van Cauwenberge, P., & Williams, H. C. (2004). Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. The Journal of allergy and clinical immunology, 113(5), 832–836. https://doi.org/10.1016/j.jaci.2003.12.591
- Lee, H. K., & Reiche, L. (2023, July). Topical corticosteroid withdrawal. Reviewed by I. Coulson. Retrieved July 15, 2023, from https://dermnetnz.org/topics/topical-corticosteroid-withdrawal
- Lio, P. A., & Bhattacharya, T. (2014). A Long View: Conceptions of Atopic Dermatitis Through the Ages. Clinical Focus. Retrieved July 15, 2023, from https://practicaldermatology.com/articles/2014-dec/a-long-view-conceptions-of-atopic-dermatitis-through-the-ages
- National Eczema Association. (n.d.). Eczema facts. Retrieved July 15, 2023, from https://nationaleczema.org/research/eczema-facts/
- Ngan, V., & Stewart, T. (2017, November). Cradle Cap. DermNet NZ. https://dermnetnz.org/topics/cradle-cap
- Ngan, V., & Oakley, A. (2016, February). Erythroderma. DermNet NZ. https://dermnetnz.org/topics/erythroderma
- Rapaport, M. (2015). Topical Steroid Whitepaper. https://red-skin-syndrome.com/white-paper-on-steroid-addiction/
- Rapaport, M. J., & Rapaport, V. (1999). Eyelid dermatitis to red face syndrome to cure: clinical experience in 100 cases. Journal of the American Academy of Dermatology, 41(3 Pt 1), 435–442. https://doi.org/10.1016/s0190-9622(99)70118-0
- Sheehan, M. P., Rustin, M. H., Atherton, D. J., Buckley, C., Harris, D. W., Brostoff, J., Ostlere, L., & Dawson, A. (1992). Efficacy of traditional Chinese herbal therapy in adult atopic dermatitis. The Lancet, 340(8810), 13-17. https://doi.org/10.1016/0140-6736(92)92424-e
- Stanway, A., & Jarrett, P. (2023, May). Atopic dermatitis. DermNet NZ. https://dermnetnz.org/topics/atopic-dermatitis
- Silverberg, J. I., Simpson, E. L., Durkin, H. G., & Joks, R. (2013). Prevalence of allergic disease in foreign-born American children. JAMA pediatrics, 167(6), 554–560. https://doi.org/10.1001/jamapediatrics.2013.1319
- Uzun, S., Wang, Z., McKnight, T. A., Ehrlich, P., Thanik, E., Nowak-Wegrzyn, A., Yang, N., & Li, X.-M. (2021). Improvement of skin lesions in corticosteroid withdrawal-associated severe eczema by multicomponent traditional Chinese medicine therapy. Allergy, Asthma & Clinical Immunology, 17(68). https://doi.org/10.1186/s13223-021-00555-0
- von Kobyletzki, L. B., Bornehag, C. G., Hasselgren, M., Larsson, M., Lindström, C. B., & Svensson, Å. (2012). Eczema in early childhood is strongly associated with the development of asthma and rhinitis in a prospective cohort. BMC dermatology, 12, 11. https://doi.org/10.1186/1471-5945-12-11
- Xu, Y. (2004). Dermatology in Traditional Chinese Medicine. Donica Publishing.


