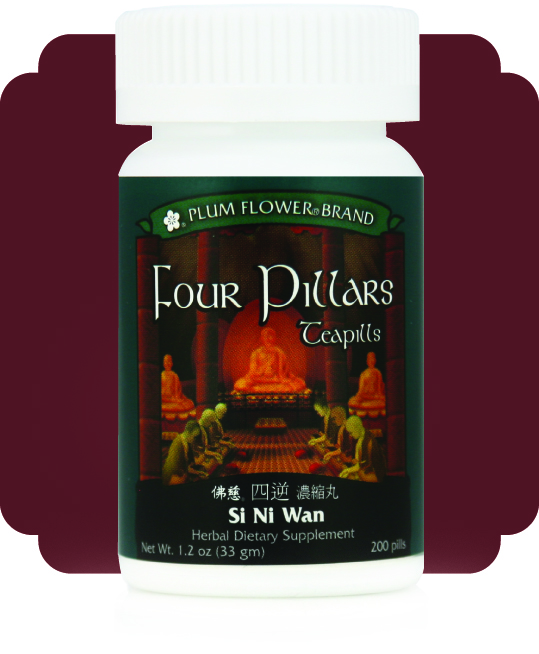
Si Ni San Wan (Four Pillars) to Release Constraint
TCM Functions: Dredges and Softens the Liver, Moves Liver Qi, Clears Heat from the Interior, Harmonizes Liver and Spleen.
TCM Diagnosis: Liver Qi stagnation with heat constrained in the interior impeding the flow of Qi to the extremities. Also for Liver Qi stagnation overacting on the Spleen and Stomach.
Presentation: Cold fingers and toes while the limbs and body remain warm. May also present with epigastric, abdominal or costal discomfort and fullness, irritability, low mood, mood swings, occasional cough, bitter taste in the mouth, poor appetite, belching, occasional nausea, occasional loose or perhaps watery stools, occasional urinary difficulty, irregular menstruation, premenstrual syndrome, teeth grinding and jaw tension. May be exacerbated by stress or emotional upset; symptoms may also manifest cyclically.
Tongue: red with a yellow coat
Pulse: wiry
Formula: Bai shao/Paeonia lactiflora root 31.5%, Chai hu/Bupleurum chinense root 26.4%, Zhi shi/Citrus aurantium fruit-immature 26.4%, Zhi gan cao/Glycyrrhiza uralensis root-prep 15.7%.
Dosage & Administration: The standard dosage is 8 pills, 3 x day. Administer half an hour before eating for optimal digestion & absorption. In the initial phases, dosage may be increased to 8-12 teapills 3 times per day, then reduced to a maintenance dose as the formula takes effect. May be used medium to long-term for several weeks to several months. Monitor for signs of Yin deficiency.
Cautions & Contraindications: Contraindicated for very weak or deficient patients. Use with caution during pregnancy. Contraindicated for cold extremities due to Kidney Yang deficiency. Contraindicated during the early stages of acute infection or illness, such as cold or flu. Use with caution in Spleen Qi deficiency.
Clinical Comments: Zhang Zhong-jing’s famous formula Si Ni San was published in the Shang Han Lun/Discussion of Cold Damage in approximately 200 A.D. Si Ni San, which translates to “Frigid Extremities Powder” treats Yang Jue, or hot type inversion, due to the internal constraint of Yang Qi. The classical symptom of cold fingers and toes while the body remains quite warm - as opposed to the whole hands and feet or even the whole limbs being cold - indicates that the cold is not due to true cold but rather to constraint. Although originally designed to treat Yang Jue constraint due to an external pathogen progressing from the Shaoyang to the more interior Shaoyin level and blocking the flow of Liver and Gall Bladder Qi, in modern practice we most frequently see patients with this presentation due to long-term Liver Qi stagnation, which over time generates smoldering heat in the trunk that constrains and prevents the Yang Qi from flowing to the extremities to warm them.
The primary goal of the formula is to invigorate the flow of Liver Qi and vent the smoldering heat, and thus to open the flow of Yang Qi to the extremities. Because the formula strongly invigorates the flow of Liver Qi, later generations of physicians expanded the use of the formula to harmonize the Liver and Spleen and alleviate digestive symptoms due to the Liver invading the Spleen. Si Ni San is now famous for being the formula upon which all other formulae to invigorate the flow of Liver Qi are based.
In the modern clinic, Si Ni San is used for Liver Qi stagnation patterns with cold extremities, stress, emotional upset and digestive disturbance. Key symptoms include digestive issues in a patient with cold hands and feet where the cold is usually limited to the fingers and toes and doesn’t extend past the wrists or ankles, symptoms are worsened by strong emotions and stress, and are accompanied by a wiry pulse and a red tongue.
Chai hu, the chief herb in the formula, strongly vents heat and releases constraint to invigorate the flow of Liver Qi. It vents and guides pathogens outwards in the case of a Shaoyin level disorder. Chai hu’s strong Qi movement aids the ascent of clear Yang and the descent of turbid Yin. It harmonizes the Liver and Spleen by reducing the excessive sideways movement of stagnant Liver Qi overacting on the Spleen. Zhi shi activates and breaks up stagnant Qi and reduces accumulation in the middle jiao to unburden and aid the Spleen in its function to transform food and transport fluids. The strong upward movement of Chai hu coupled with the equally strong downward movement of Zhi shi quickly re-establishes the free movement of Qi to restore the Qi dynamic and relieve the constraint. Bai shao nourishes Liver Blood, preserves the Yin, softens the Liver and moderates the drying and dispersing nature of Chai hu. Bai shao combines with Zhi gan cao as in Shao Yao Gan Cao Tang to nourish the sinews and calm spasms to alleviate digestive symptoms, particularly spasmodic issues, due to Liver invading the Spleen. Zhi gan cao tonifies the middle jiao and strengthens Qi to aid the Spleen in its transformation and transportation functions.
Combinations: For Blood deficiency and true cold with the entire hands and feet cold, switch to Dang Gui Si Ni Tang. For Qi rebelling upwards causing occasional heartburn, may be administered with Xiang Lian Wan. For Qi stagnation with damp-heat accumulating in the Gall Bladder, may be combined with Li Dan Pian. For food stagnation creating more marked digestive distress, may be combined with Bao He Wan.
References:
- The Clinical Manual of Chinese Herbal Patent Medicines, 3rd Edition, by Will Maclean with Kathryn Taylor, Pangolin Press, 2016.
- Chinese Herbal Medicine - Formulas and Strategies, 2nd Edition, by Dan Bensky, Volker Scheid, Andy Ellis and Barolet, Eastland Press, 2009.
- Chinese Herbal Medicine – Materia Medica, 3nd Edition, by Dan Bensky, Steven Clavey and Erich Stoger, with Gamble, Eastland Press, 2004.
- Chinese Herbal Formulas and Applications - Pharmacological Effects & Clinical Research, by John Chen & Tina Chen, Art of Medicine Press, 2009.
- Chinese Medical Herbology and Pharmacology, by John Chen & Tina Chen, Art of Medicine Press, 2004.
- 160 Essential Chinese Herbal Patent Medicines, by Bob Flaws, Blue Poppy Press, 1999.


