Osteoporosis and TCM
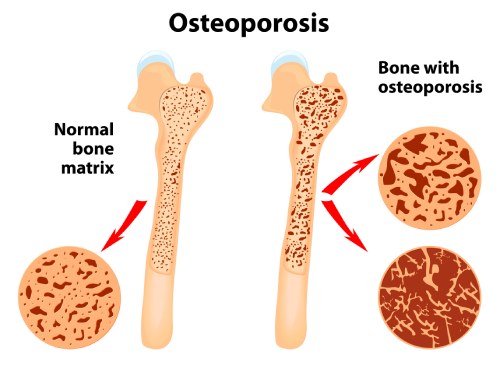
First defined in 1993, osteoporosis (lit. “porous bone”) is a skeletal disorder characterized by low bone mass with deterioration and loss of bone tissue which is accompanied by additional bone porosity, a decrease in bone density, bone frailty, and increased fracture risk. Osteoporosis is the most common reason for broken bones among the elderly, and it is estimated that more than 200 million people worldwide suffer from this condition. Often precipitated by a fall, the bones that commonly break include the spinal vertebrae, or bones of the proximal humerus, ribs, forearm, wrist, and hip (possibly the most disabling). While these fractures, and osteoporosis, occur in both women and men, they become prevalent in women after 55 years of age, while they occur in men mostly after 65. Although the risk factors are similar, the etiologies of osteoporosis in males are divergent. This article will focus on osteoporosis in women.
Any event that can reduce bone formation or increase bone resorption can lower the bone mineral density (BMD) and when the BMD is below 2.5 standard deviations from that of a young adult, osteoporosis is defined. BMD is measured using low levels of x-rays in an imaging test called dual-energy X-ray absorptiometry (DEXA). A BMD not quite reaching this threshold may be defined as osteopenia, meaning a deficiency in bone density (sometimes it may mean deficiency in bone mass). Bone density reaches its peak at 30-36 years of age, and because the osteoporosis threshold is rarely experienced during pre-menopause, osteoporosis is associated with aging. This correlates with the observation that the deterioration of bone structure maintenance is a result of several aging factors, even though bone loss begins well before menopause and accelerates during perimenopause.
Bones are not inert structures within the human body; they continue to change over the course of a person’s lifespan. The human skeleton is completely renewed about every 10 years through a process called bone remodeling, which serves to protect the structural integrity of the skeletal system and to metabolically contribute to the body's balance of calcium and phosphorus. Remodeling first entails the resorption of old or damaged bone by cells called osteoclasts, which reabsorb mineralized bone before they undergo apoptosis. Coincidentally, osteoblasts (literally, “bone germinating”) are recruited from stem cells, at the same site, to make and mineralize new bone tissue. During growth and development, there is a quantitative balance between the amount of bone formation and resorption. As one ages, due to fluctuations in the hormonal controls governing temporal and spatial processes, the bone remodeling process can become disrupted.
It is generally true that bone loss increases after menopause due to lower levels of estrogen, and in older men due to lower levels of testosterone. However, osteoporosis may also occur due to various diseases or medical interventions, including alcoholism, anorexia, bulimia, hyperthyroidism, kidney disease, and surgical removal of the ovaries (ovariectomy). Certain medications increase the rate of bone loss, including some antiseizure medications, chemotherapy, proton pump inhibitors, selective serotonin reuptake inhibitors, and glucocorticosteroids. Smoking, a poor diet (especially lacking in calcium and phosphorus), and too little exercise are also risk factors.
Estradiol (E2) is women's dominant bone hormone since it is essential for development of adolescent peak bone mineral density and the presence of adequate physiological levels of estrogen prevent bone resorption that causes most adult BMD loss. During the luteal phase, E2 decreases, triggering bone resorption and then progesterone, which initially rises during the progression of the developing follicle, serves to increase progesterone-receptor-mediated, slow osteoblastic bone formation that modulates the potential loss of bone density. When menstrual cycles are normal length and normally ovulatory, estradiol and progesterone are “balanced”, and BMD is stable.
Although progesterone is produced by males and females by the cortex of the adrenal glands, the corpus luteum produces relatively larger amounts of progesterone to nourish the implanted follicle during a woman’s cycle. If the egg becomes fertilized, the progesterone levels in the mother climb precipitously because the embryo needs a lot of progesterone since it is the precursor for all cortical steroid hormones. If the egg is not fertilized, the follicle and the corpus luteum degenerate and consequently, the progesterone level falls to baseline, which induces the uterine lining to shed along with the remnants of the unfertilized follicle, corpus luteum and blood supply that constitute the menses.
Unfortunately, many women commonly have ovulatory disturbances characterized by irregular cycles, amenorrhea, anovulation, and short luteal phases with the consequence of low progesterone levels since when there is no ovulation, there is no follicle released. This results in low levels of progesterone available for mitigating bone resorption during the menstrual cycle. These ovulatory disturbances are more frequent in teen and perimenopausal women and are increased by everyday stressors: energy insufficiency, emotional/social/economic threats, excessive athletic activity and lack of quality sleep. Issues such as obesity, disordered eating patterns like anorexia or bulimia and other conditions such as polycystic ovary syndrome (PCOS) can also contribute. Research suggests that almost 1%/year spinal BMD loss occurs in those with greater than median (∼31%) of ovulatory disturbed cycles.
While the advent of decreased sex hormones is implicated, several other endocrine hormones and systems governed by hypothalamic-pituitary-gonadal function, all of which also vary with age, diet, and life-style choices, can play a role in the development of osteoporosis.

While the rise in thyroid-stimulating hormone (TSH) levels is protective to bone mass, the decline of estrogen, testosterone, insulin-like growth factor 1 (IGF1), and vitamin D as well as the rise of cortisol, parathyroid hormone, and follicle stimulating hormone (FSH) can contribute to bone loss in the elderly. Particularly, the estrogen serum level decrease and the consequent FSH increase enhance bone resorption, whereas the decline of testosterone and IGF1 negatively impact bone formation. Even though it has been reported that vitamin D has a direct effect on osteoblastogenesis, i.e., the creation of osteoblasts, low levels of vitamin D mainly impacts bone metabolism due to the rise of parathyroid hormone levels, which, in turn, induces osteoclastogenesis; the net result being loss of bone density. In adults, when there is a deficiency of vitamin D and inadequate levels of phosphate and calcium, this is called osteomalacia, which is characterized by the “softening” of the bones from impaired bone metabolism, which in turn causes inadequate bone mineralization. Additionally, the release of proinflammatory cytokines by T-cells of the immune system and osteoblasts seem to accelerate bone reabsorption.
Biomedicine treatment is based on an assessment of one’s risk of experiencing a fall or a bone fracture within ten tears by measuring bone density and one’s age. If the risk is low, then there may be a focus on increasing calcium and vitamin D intake from diet with supplementation of these nutrients, if necessary, along with exercise including weight bearing and balance exercises. Since systemic magnesium deficiency is difficult to assess from blood tests, magnesium deficiency might affect bone directly by reducing bone stiffness, increasing osteoclasts, and decreasing osteoblasts and indirectly by interfering with parathyroid hormone and vitamin D, which promotes inflammation/oxidative stress and subsequent bone loss. Additionally, many adults do not obtain sufficient magnesium from diet, and supplementation of this mineral may be indicated. When medications are deemed necessary, bisphosphonates, parathyroid hormone mimics, or a monoclonal antibody may be prescribed, all of which have been shown to increase bone density although there are several adverse effects that must be considered.
In Western biomedicine, hormone related therapy (HRT) involving estrogen is commonly recommended, especially when it is begun once a woman is showing signs of approaching menopause. However, oral supplemental estrogen can increase the risk of breast cancer, blood clots, and stroke and consequently adding progesterone to HRT has become part of the standard of care. Progesterone treatment is also often prescribed for the teen-to-perimenopausal recurrent cycle/ovulatory disturbances. Progesterone plus estradiol or other antiresorptive therapies adds bone density of 0.68%/year, which represents a significant slowing of BMD loss.
Until recently, the principal form of progesterone was medroxyprogesterone (Povera™), a synthetic progestin. The adverse effects and warnings that accompany synthetic progestins have resulted in this approach to only be used with caution. The numerous adverse effects of medroxyprogesterone include an increased risk of blood clots, stroke, and heart attack, et al. (see list here.) Orally administered estradiol and progesterone require relatively high doses because these drugs are subject to the first-pass effect in the liver. Instead, IV allopregnanolone (a metabolite of progesterone, sold as Zulresso™), oral micronized progesterone (known as “cyclic” since it is only taken during a part of the month, sold as Prometrium™ but available generically), or transdermal USP progesterone creams (such as Emerita Pro-gest™, et al.) are recommended. There is also evidence that low-dose transdermal or vaginal estrogen cream avoids many of the adverse effects of oral forms, although the risks are not entirely eliminated.
TCM Perspectives
In traditional Chinese medicine (TCM), the responsibilities of endocrine hormones, development, maturation, and aging are primarily given to Kidney Jing, although the correct functioning of the various systems of the body are also dependent on Qi, Blood, and Shen. Lifestyle choices, diet, exercise, and adequate sleep are also necessary to maintain harmony with the Dao. (See our article “Longevity, TCM and The Hallmarks of Aging”. ) Consequently, Chinese herbal formulas for the therapy of osteoporosis contains a variety of herbal medicines, which can primarily be divided into three categories based on their action in the formula: (1) replenishing the Kidney Yin and/or Yang, as appropriate, thereby supporting the Kidney Jing (Essence); (2) tonifying the Spleen to augment Qi and Blood; (3) moving Qi and Blood and dissipating Blood stasis.
Quite a bit of research has been conducted into the effects of Chinese herbs on bone density involving over one hundred herbs. Peng, et al., includes a chart listing 30 herbs and references to both in vivo and in vitro studies, a link to which can be found in the reference section. Here are some of the highlights of research into the use of Chinese herbs to support healthy bone density.
Herba Epimedii
The dried aerial component of various Epimedium species known as (Yin yang huo) belongs to the Tonify the Kidney Yang category in TCM. Flavonoids, phenolic glycosides, ligans, penethylol glycosides, ionones and sesquiterpenes have all been extracted from Epimedium species, and Epimedium is among the most recommended herbs for TCM osteoporosis formulations. Yin yang huo, either as a solo herb or in an herb formula, has been shown to prevent or inhibit bone resorption, enhance E2 levels, and lower systemic IL-6 levels (a pro-inflammatory cytokine secreted by osteoblasts to stimulate osteoclast formation). Icariin is the major bioactive flavonoid glucoside extracted from Epimedium and it is linked to the herb’s pharmacological activities. In one in vitro study, treating Yang deficiency, Epimedium polysaccharides improved bone cell multiplication by 72% and DNA replication of bone marrow cells was enhanced by 68%.
Drynaria Rhizome
The dried rhizome of the perennial Drynaria fortunei is known as Gu sui bu and is another Kidney Yang tonic. The literal English translation for this herb is “mender of shattered bones” and it is often used to treat musculoskeletal diseases in traditional Chinese medicine. Gu sui bu also possesses anti-osteoporosis properties supported by research finding that it inhibited ovariectomy-induced bone resorption and it has a powerful blocking action on cathepsin-K induced decomposition of collagen via reducing cathepsin-K activities. (Cathepsin-K is a protease enzyme that promotes bone remodeling and resorption.) Furthermore, naringin is a flavonoid with estrogenic action that is found naturally in Drynaria fortunei as bioactive component. Naringin enhances the growth and osteoblast development of bone mesenchymal stem cells and induces osteogenesis through stimulating estrogen receptor phosphorylation in osteocytes. Gu sui bu’s main positive activity on bone cells seems to include the triggering of apoptosis in osteoclast cells.
Curculigo Rhizome
In Chinese medicine, Curculigo orchioides (Xian mao), has been applied topically for the management of knee and spine joint arthritis, leg fatigue and diarrhea. Xian mao is also a Yang tonic herb, which is seen to have antioxidant, antiosteoporotic, and antitumor effects. In a research study, Curculigo reduced bone degradation in tibias by reducing osteoclast activity and boosting serum calcium, phosphorus, and oocyte levels while having no effect on uterus size. Xian mao might stimulate bone regeneration after the healing process due to its principal biologically active component, curculigoside, a phenolic glycoside, which is reported to have antiosteoclastic and osteogenic properties.
Fructus Ligustri Lucidi
Fructus Ligustri Lucidi (Nu zhen zi) is used to tonify the Kidney and Liver Yin and augment the bones as a singular herb. In ovariectomized rats Nu zhen zi enhanced bone density and bone’s mechanical integrity. Additionally, Ligustri modulates calcium equilibrium in older women by modifying the parathyroid-vitamin-D axis and increasing absorption of calcium in vivo, implying that Fructus Ligustri might be an appropriate therapy for restoring calcium and vitamin-D equilibrium. Oleanolic acid, the significant bioactive compound in Nu zhen zi enhanced the osteoblastic delineation of osseous mesenchymal stem cells and osteoprotective activity in ovariectomy-induced osteoporotic rats in vitro.
Eucommia Ulmoides Cortex
Eucommia Ulmoides (Du zhong) is a Kidney Yang tonic herb that has been reported to inhibit osteolysis and bones density depletion, as well as stimulate osteogenesis. The phytochemicals in Eucommia play an active role in every sequence of the pathways for initiating osteoblasts to expedite osteogenesis and impeding osteoclast action and block osteolysis. The oral administration of Du zhong was found to prohibit the degradation of trabecular micro-architecture of the tibia and loss of estrogen deficiency-induced osseous micronutrients. Interestingly, Eucommia extracts have been reported to activate the secretion of growth hormone, which controls bone growth, development, and bone formation, implying that Du zhong could be a promising candidate for the treatment of osteoporosis.
Fructus Psoralea
The dehydrated mature fruits of the perennial herb Psoralea corylifolia (Bu gu zhi) is also listed among herbs that are used to tonify the Kidney Yang. An extract of Bu gu zhi was found to promote bone regeneration through increasing bone mineralization and serum inorganic phosphorus, which indicate components of the herb could be effective treatments for osteomalacia, osteoporosis, broken bone, and other skeletal disorders. Psoralea preparations stimulated osteoblastic development in vitro. The flavonoids bavachin and corylin have been recovered from Bu gu zhi and defined as bioactive components.
Herba Eclipta prostrate
The aerial components of Eclipta prostrata (Han lian cao) are used in Chinese herbal medicine to nourish and tonify the Kidney and Liver Yin, cool the Blood, and stop bleeding. Ecliptae herba produces the chemical wedelolactone, which has been shown to improve bone marrow stem cells development into osteoblasts. The extract was given orally as well as applied topically on fractured sites. When bone marrow stem cells are incubated with wedelolactone, the production of alkaline phosphatase, a diagnostic enzyme for mature osteoblasts, increases in a dose-dependent way. In addition, wedelolactone caused an elevation in bone’s calcification. The expression of genes associated with osteoblastogenesis was elevated. Wedelolactone treatment to ovariectomized rats reduced ovariectomy induced bone resorption by increasing osteoblast activation and stimulating osteogenesis.
Radix Salvia miltiorrhiza
Salvia miltiorrhiza (Dan shen) is used in Chinese herbal medicine to nourish and invigorate the Blood, dispel Blood stasis, and calm Shen. The anti-osteoporotic effect of Salvia miltiorrhiza is ascribed to its TCM action on Liver and Blood stasis as the main therapeutic targets defining osteoporosis. Researchers have investigated the anti-osteoporotic potential of Dan shen in at least thirty-six investigations in contrast to Western medications including vitamin D2, caltrate, alendronate, and calcitonine, and bisphosphonate with the reported result of a considerable benefit in boosting bone mineral density. More than 100 individual compounds have been isolated from Dan Shen and tested in various animal models and biochemical assays. Compounds display anti-resorptive and bone formation-stimulating features targeting different pathways in the bone remodeling cycle. Pathways affected include the activation of osteoblasts, the modulation of osteoclastogenesis, and the inhibition of collagen degradation by cathepsin K.
Radix Rehmannia
Rehmanniae Radix/ Shu di huang exerts the anti-osteoporotic effect via regulating the functions of Kidney and Liver as well as improving blood circulation. Shu di huang has been the subject of numerous clinical trials in combination with other herbs to treat post-menopausal, senile, and secondary osteoporosis. Most of the clinical trials are characterized by high efficacy with no obvious adverse effects. More than 140 individual compounds have been isolated from Rehmannia and many have been reported to show pleiotropic (gene expression) effects on various diseases. The pharmacokinetics data demonstrate catalpol and ajugol as well as acetoside are the active constituents. Rehmanniae Radix displays bone protecting features in the osteoporosis models via the delicate balance between osteoclastogenesis and osteoblastogenesis through single herb extracts and its isolated compounds.
Rhizome Atractylodes macrocephala
Atractylodes macrocephala / Bai zhu is used in traditional Chinese herbology to tonify the Spleen and Stomach Qi. Research has discovered that Bai zhu inhibits osteoclast differentiation from its precursors induced by receptor activator of nuclear factor-κB ligand, an essential cytokine required for osteoclast differentiation, and subsequently inhibiting the induction of osteoclastogenic transcription factors. Atractylenolide I and II are the active constituents contributing to the anti-osteoclastogenic effect of Bai zhu. Atractylodes has a protective effect on bone loss via inhibiting osteoclast differentiation and it may be useful in preventing and treating various bone diseases associated with excessive bone resorption.
Radix Astragalus membranaceus
Astragalus membranaceus root/ Huang qi is a Chinese herb used in traditional Chinese herbology to tonify Qi and Blood, tonify the Spleen and raise the Yang Qi of the Spleen and Stomach. Extracts of Astragalus improve aging bone marrow mesenchymal stem cells (BMSCs) vitality and osteogenesis. Mesenchymal stem cells can be differentiated into nerve, muscle, and bone and they play a key role in bone formation and repair. In patients with osteogenesis insufficiency, BMSCs activation would promote bone growth, improve bone content, and reduce the incidence of breaks. The differentiation ability of BMSCs decreases with aging, consistent with osteoporosis development. Research suggests that Huang qi can improve the aging BMSCs vitality and bone formation by the regulation of vitamin D and the vitamin D receptor used to promote BMSCs into osteoblasts.
Radix Angelica sinensis
Angelica sinensis root/ Dang gui is a Chinese herb traditionally used to tonify the Blood and regulate the menses. Dang gui is one of the most commonly used Chinese herbs for the treatment of osteoporosis and in addition, it is helpful for the treatment of osteoarthritis. Studies have confirmed that rats treated with Angelica sinensis showed less trabecular bone loss and thicker cortical areas. The volatile oil is one of the main effective components of Dang gui, and ligustilide is the most abundant component in the volatile oil. Ligustilide has been found to have multiple pharmacological activities such as anti-atherosclerosis, neuroprotection, anti-cancer, inhibition of cardiac hypertrophy, anti-inflammation, and analgesia, and in addition, has been reported to protect skeletal muscle cells, nerve cells, and endothelial cells from various sorts of damage. Research has shown that ligustilide regulates bone formation and increases bone mass, promotes osteoblast differentiation, and prevents premature osteoblast apoptosis. Among the known constituents of Dang gui is a chemical called Angelica polysaccharide (AP). AP promotes proliferation and osteoblast differentiation in mesenchymal stem cells (MSCs). AP upregulates the expression level of H19 (H19 is a gene for a long noncoding RNA, which has a role in the negative regulation of body weight, cell proliferation, and gene expression in MSCs.) This polysaccharide promotes osteoblast differentiation and bone formation in vivo.
Er-Xian Tang
Two Immortals Decoction/Er-Xian Tang is a multi-herb composition consisting of Epimedium and Curculigo plus four other herbs: Herba Epimedii/Yin yang huo (9-15g), Rhizome Curculiginis/Xian mao (6+15g), Cortex Phellodendri/Huang bai (4-9g), Radix Morindae officinalis/Ba ji tian (6-9g), Radix Angelicae sinensis/Dang gui (6-12g), and Rhizome Anemarrhenae/Zhi mu (4-6g). Traditionally, it is used to replenish Kidney Yin and Yang, tonify Kidney Jing, purge deficiency Fire, and regulate disharmony of the Chong and Ren, which speaks to its use in gynecological conditions where there is an imbalance of sexual hormones.
Er Xian Tang/San has proven effective in reducing osteoporosis, perimenopausal syndrome, and other issues that may present in older patients. Two Immortals Decoction is therapeutically useful in alleviating menopausal symptoms by boosting the level of circulating estradiol as well as increasing antioxidant and endocrine activity through the stimulation of catalase and aromatase detoxification channels. This formula has been proven to have anti-osteoporotic actions comparable to estrogens and has attributed enormously to the prophylaxis or therapy of bone loss caused by ovariectomy. It has beneficial benefits on bone while having just minimal impact on the uterus, demonstrating that Er Xian Tang is acceptable to be used for bone health management.
Final Thoughts
Remember, the onset of osteoporosis occurs in early middle age long before any observable symptoms develop. Diet, chemical exposures, illnesses, stress, emotional imbalances, lifestyle choices involved in over-doing and over-thinking, and lack of exercise are important factors to consider in order to decrease the risk of developing this condition. For both men and women, living in harmony with the Dao by finding and maintaining the balance of Yin and Yang is critical for health and longevity. For women, the frequency of irregular menses and anovulatory cycles point to a need to address these issues as early as possible in a woman’s life to create balance, harmony, and regularity with the dance of the gonadal steroids. Establishing such a balance will conserve the Jing and serve to slow the natural aging processes that include a deterioration in bone remodeling. Fortunately, there are Chinese herbal medicine remedies that can mitigate the TCM syndromes caused by the disharmonies and challenges of life and that can, at least, slow down this aspect of the aging process.
Resources
- Bensky, D. & Barolet, R., Formulas & Strategies, Eastland Press: 1990.
- Bensky, D. et al., Chinese Herbal Medicine Materia Medica, 3rd ed., Eastland Press: 2004.
- Cannarella, R., et al., “Osteoporosis from an Endocrine Perspective: The Role of Hormonal Changes in the Elderly”, Journal of Clinical Medicine: Oct 2019, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6832998/
- Che, T., et al., “Natural Products from Chinese Medicines with Potential Benefits to Bone Health”, Molecules: Feb 2016, https://www.mdpi.com/1420-3049/21/3/239
- Cheng, M. & Gupta, V., “Premenopausal osteoporosis”, Indian Journal of Endocrinology & Metabolism: Mar 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3683197/
- Guo, Y., et al., “Salvia miltiorrhiza: an ancient Chinese herbal medicine as a source for anti-osteoporotic drugs”, Journal of Ethnopharmacology: Sep 2014, https://pubmed.ncbi.nlm.nih.gov/25109459/
- Ha, H., et al., “Ethanol Extract of Atractylodes macrocephala Protects Bone Loss by Inhibiting Osteoclast Differentiation”, Molecules: Jul 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6269826/
- Lee, J., Natural Progesterone: The Multiple Roles of a Remarkable Hormone, BLL Publishing 1993.
- Liu, C. et al., “Rehmanniae Radix in osteoporosis: A review of traditional Chinese medicinal uses, phytochemistry, pharmacokinetics and pharmacology”, Journal of Ethnopharmacology: Feb 2017, https://pubmed.ncbi.nlm.nih.gov/28111216/
- Mayo Clinic Staff, “Osteoporosis”, Mayo Foundation for Medical Education and Research, https://www.mayoclinic.org/diseases-conditions/osteoporosis/symptoms-causes/syc-20351968
- Mills, E., et al., “The Relationship Between Bone and Reproductive Hormones Beyond Estrogens and Androgens”, Endocrine Reviews: Dec 2021, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8599211/
- Peng, Z. et al., “Role of Traditional Chinese Medicine in Bone Regeneration and Osteoporosis”, Frontiers in Bioengineering and Biotechnology, Tissue Engineering and Regenerative Medicine Volume 10 – 2022, https://www.frontiersin.org/articles/10.3389/fbioe.2022.911326/full
- Prior, JC, “Progesterone for the prevention and treatment of osteoporosis in women”, Climacteric: Aug 2018. https://pubmed.ncbi.nlm.nih.gov/29962257/
- Prior, JC, “Cyclic Progesterone Therapy”, Center for Menstrual Cycle and Ovulation: Dec 2018, https://cemcor.ubc.ca/resources/cyclic-progesterone-therapy
- Pu, X., et al., “Astragalus improve aging bone marrow mesenchymal stem cells (BMSCs) vitality and osteogenesis through VD-FGF23-Klotho axis”, International Journal of Clinical & Experimental Pathology: Apr 2020, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7191145/
- Puckey, M. (rev), “Medroxyprogesterone”, Drugs.com, Cerner Multum, Inc., 2024, https://www.drugs.com/medroxyprogesterone.html#side-effects
- Rondaanelli, M., et al., “An Update on Magnesium and Bone Health”, Biometals: May 2021, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8313472/
- Rosenfield, R., “Adolescent Anovulation: Maturational Mechanisms and Implications”, Journal of Clinical Endocrinology & Metabolism: Aug 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3763969/
- Rowe, P., et al., “Physiology, Bone Remodeling”, StatPearls: Mar 2023, https://www.ncbi.nlm.nih.gov/books/NBK499863/
- Wang, Z. et al., “Chinese Herbal Medicine for Osteoporosis: A Systematic Review of Randomized Controlled Trials”, Evidence-Based Complementary and Alternative Medicine 2013. https://www.hindawi.com/journals/ecam/2013/356260/
- Xie, X., et al., “Angelica polysaccharide promotes proliferation and osteoblast differentiation of mesenchymal stem cells by regulation of long non-coding RNA H 19”, Bone & Joint Research: Aug 2019 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6502875/
- Zhang, DZ, et al., “Traditional Chinese medicine formulas for the treatment of osteoporosis: Implication for antiosteoporotic drug discovery”, Journal of Ethnopharmacology: Aug 2016, https://www.sciencedirect.com/science/article/abs/pii/S0378874116302975