Case Study: Treatment for “Fen Ci” (粉刺) with TCM
Chinese herbal medicine can be very helpful to control one of the most common skin conditions in the world, known in traditional Chinese medicine as Fen Ci (粉刺) or “white thorns”, which can have a variety of etiologies. Modern medicine offers many pharmaceutical treatments, all of which can have potential side effects. Traditional Chinese herbal medicine provides a natural alternative to those harsh chemicals, and with little to no side effects. In my clinical experience, this can be a stubborn condition to treat and oftentimes, the patient will experience little change during the first 5 to 6 months of treatment, so it takes extraordinary patience and commitment on their part. In this article, I present a case of adult acne, as diagnosed by her dermatologist, in an American 24-year-old cis female of Chinese heritage.
Acne is known in traditional Chinese medicine as Fen Ci “white thorns”, or Fei Feng Fen Ci (肺風粉刺) “lung wind white thorns” and while these names indicate that the comedones are white or due to wind, that is not always the case. Comedones can appear pink, red, purple or dark brown in color, depending on the skin tone of the patient and the pattern of disharmony. As usual, Chinese herbal medicine treatment is based on pattern differentiation. The pathological origins of Fen Ci (粉刺) can be due to a singular or combined pattern of Damp Heat, Stomach Heat, Liver-Spleen disharmony, dysregulation of the Chong and Ren meridians, Blood Stasis and more.
The patient was already under my care with acupuncture and herbs for menstrual irregularity, PMS, and stress. At this point in her treatment, the menstrual irregularity was largely resolved, and she was coming in about every three weeks for maintenance and stress reduction. In general, she still experienced some measure of PMS with irritability, breast tenderness and mild to moderate menstrual cramps.
 During the approach of her final term of her Master’s degree program, her face broke out. She was very embarrassed by the look of her skin, was under significant stress, not sleeping well, eating out a lot, and not making quality dietary choices. She also continued to experience PMS with irritability, breast tenderness, mild to moderate menstrual cramps on the first day or two and was prone to Damp Heat type vaginal yeast infections. Her bowel movements were somewhat irregular and relatively dry, and she would occasionally skip a day. She also experienced occasional painful gas in the epigastric area of her abdomen. Her tongue was red with a thick, slightly yellow coating, scalloping on the sides and the pulse was wiry. The papules were red, closed comedones on her cheeks, some of which were painful, and I observed background erythema. The skin was sebaceous, and the oiliness worsened in the afternoon. The papules would resolve as post inflammatory hyperpigmented light brown macular lesions.
During the approach of her final term of her Master’s degree program, her face broke out. She was very embarrassed by the look of her skin, was under significant stress, not sleeping well, eating out a lot, and not making quality dietary choices. She also continued to experience PMS with irritability, breast tenderness, mild to moderate menstrual cramps on the first day or two and was prone to Damp Heat type vaginal yeast infections. Her bowel movements were somewhat irregular and relatively dry, and she would occasionally skip a day. She also experienced occasional painful gas in the epigastric area of her abdomen. Her tongue was red with a thick, slightly yellow coating, scalloping on the sides and the pulse was wiry. The papules were red, closed comedones on her cheeks, some of which were painful, and I observed background erythema. The skin was sebaceous, and the oiliness worsened in the afternoon. The papules would resolve as post inflammatory hyperpigmented light brown macular lesions.
The Chinese medical diagnosis was Damp Heat with Blood Stasis. The treatment principle was to clear Heat, resolve toxicity, eliminate Damp, and invigorate the Blood to dispel Blood Stasis. This assessment was based on how the acne looked, menstrual history, and poor dietary habits, which included over-eating of dampening and sometimes greasy food leading to hindered transformation and transportation function of the Spleen. The resultant Dampness blocked the dermal layer. Damp Heat can increase sebum. Blood Stasis and Liver Qi Stagnation lead to heat in skin and obstruct the collaterals. Heat can manifest on the skin, and combined with Blood Stagnation, result in red papules and erythema.
I did not use a traditional formula. Instead, I wrote an herbal formula from scratch that is based upon several different formulas, and what I have learned from my dermatology teacher who does not use traditional formulas. This formula contains sometimes overlapping elements of: Chu Shi Jie Du Tang (Eliminate Dampness and Relieve Toxicity Decoction), San Pi Xiao Cuo Tang (Three Cortex Acne Eliminating Decoction), Xiao Yao San (Bupleurum and Dang Gui Powder), and Shao Yao Tang (White Peony Formula).
The prescription was formulated based on whole herbs, which was then converted by the dispensary to an extract granule powder. The dosage for this patient, who historically has responded well to lower dosages, was 8 grams twice per day. I thought we’d start with a pebble and see the ripple it made.
Formula Explanation:
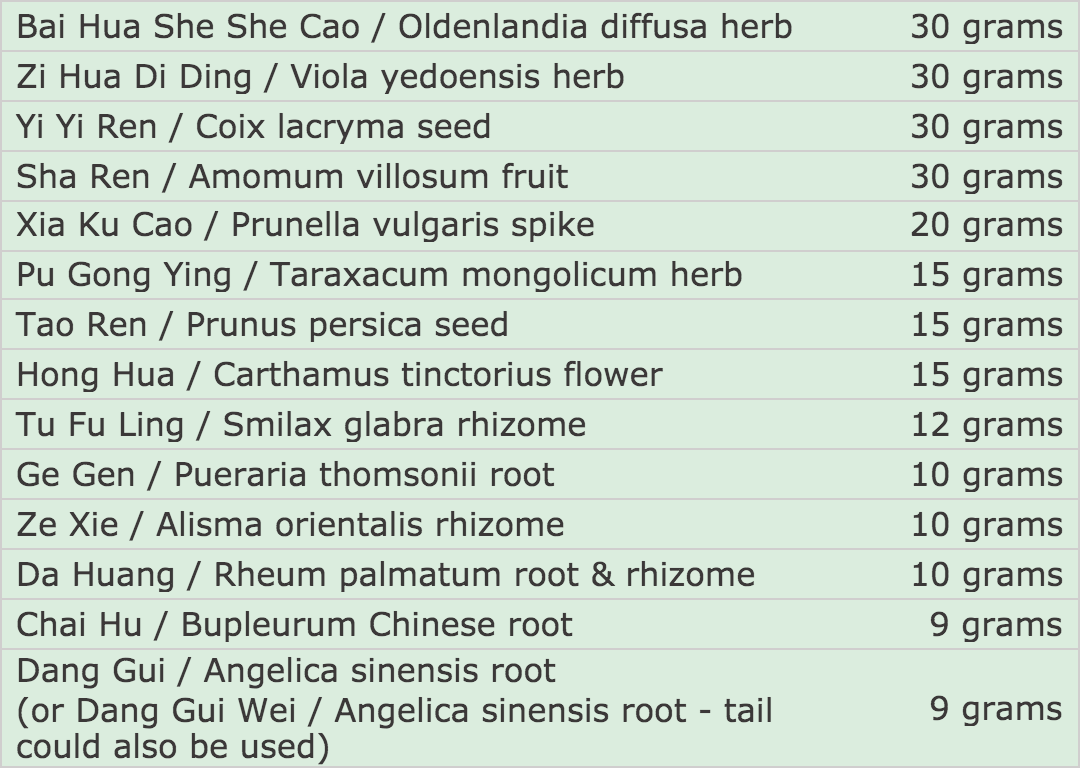
- Bai Hua She She Cao, Pu Gong Ying, Zi Hua Di Ding clear toxic Heat.
- Xia Ku Cao, Zi Hua Di Ding, Bai Hua She She Cao resolve toxins, clear hot sores, soften and dissipate nodules.
- Xia Ku Cao reduces Liver Fire, disperses Qi Stagnation and congested Heat, gently nourishes the Liver Blood, and dissipates nodules due to accumulation of Heat and Phlegm.
- Chai Hu guides the formula up to the head, spreads the Liver and relieves stagnation.
- Hong Hua, Dang Gui and Tao Ren invigorate the Blood and break stagnation.
- Tao Ren and Da Huang unblock the bowels and guide heat out via the stool.
- Tu Fu Ling, Yi Yi Ren clear Damp Heat from the skin.
- Yi Yi Ren and Sha Ren fortify the Spleen and transform Dampness.
- Yi Yi Ren is a very effective medicinal to clear sebum, expel pus and Damp Heat.
- Sha Ren regulates the Qi of the intestine, promotes bowel movements and relieves intestinal abdominal pain.
- Tu Fu Ling and Zie Xie promote urination, and lead Dampness and Heat out through the urine.
- Ge Gen relieves Heat, and vents toxic sores. While it is unusual for TCM dermatologists to use this herb, I have found it clinically effective in a variety of dermatological cases for its capability to vent toxic sores, and because it clears Wind-Heat in the upper body.
The first two weeks she failed to take the formula twice per day, so there was no improvement. Once she began taking the herbs as recommended, her skin responded very quickly. Within one month, the size of the papules was reduced and the red color began to lighten up. She had one premenstrual break out, but it manifested in fewer red papules, which resolved a bit faster. Her menstrual cycle lengthened from 24 days to 27 days and she only bled for 4 days. This indicated that the Heat was clearing, the Dampness was resolving and the Blood and Qi were beginning to flow uninhibited.
After another month, her skin was almost completely clear except for a few surface level closed comedones that were close to her normal skin tone, as well as some post inflammatory hyperpigmentation. In the months following, she would sometimes experience a premenstrual break out, or if she was under significant stress, but these eruptions were more superficial, less red, not painful and would resolve much faster.
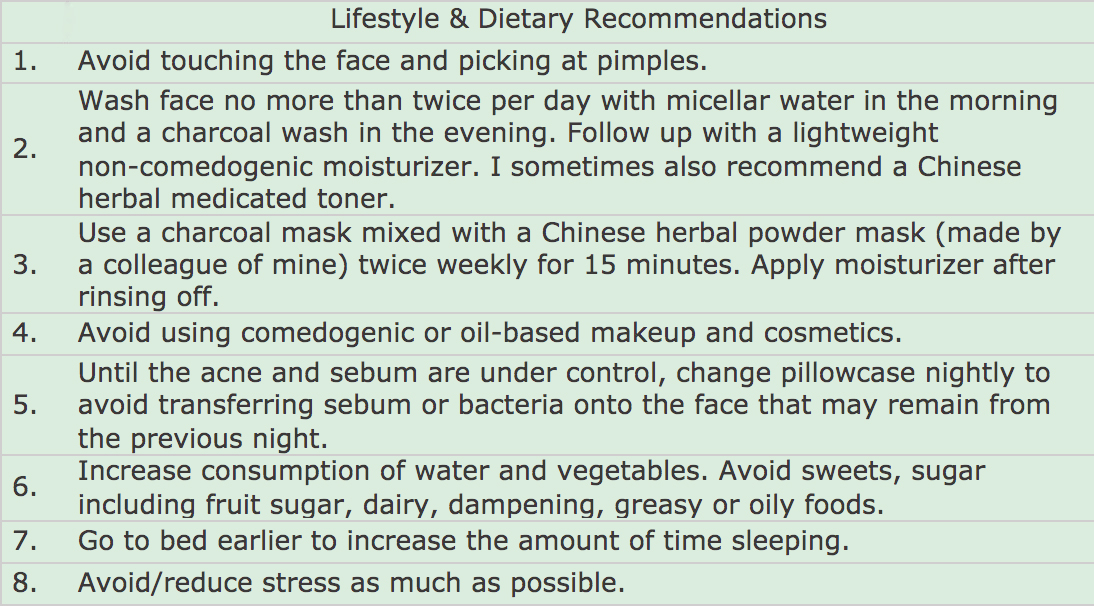 After the second month I removed the Da Huang because her bowels were moving smoothly and there was no longer a need to guide Heat out with the stool. I added 15 grams of Dan Shen / Salvia miltiorrhiza root, which is a helpful Blood mover to address hyperpigmentation and brighten the skin. She complained of increased anxiety due to looking for a job during the COVID crisis, moving to a new apartment and increased premenstrual irritability so I also added 9 grams of Bai Shao / Paeonia lactiflora root to calm Liver Yang, soften and regulate the flow of the Liver Qi and Blood.
After the second month I removed the Da Huang because her bowels were moving smoothly and there was no longer a need to guide Heat out with the stool. I added 15 grams of Dan Shen / Salvia miltiorrhiza root, which is a helpful Blood mover to address hyperpigmentation and brighten the skin. She complained of increased anxiety due to looking for a job during the COVID crisis, moving to a new apartment and increased premenstrual irritability so I also added 9 grams of Bai Shao / Paeonia lactiflora root to calm Liver Yang, soften and regulate the flow of the Liver Qi and Blood.
She remained on this version of the formula for another four months, rarely broke out and her skin looks and feels smooth with an even skin tone and most of the hyperpigmented spots are resolved. I recently sent her a final batch of this formula. When that is complete, I will give her Jia Wei Xiao Yao San as a maintenance formula to keep the Spleen and Liver Qi harmonized, to nourish and move the Blood in a gentle manner, and for its nourishing and Heat clearing qualities.
Overall, this particular case resolved much faster than most acne cases I encounter in clinical practice. Two months after we began this treatment, the COVID pandemic hit New York City, so the follow-up appointments were done remotely, via video conference, which is the method of practice I currently use for all of my cases. I examined her skin via photos that I requested she send to me. Her stress is reduced due to finding a job, a new apartment and raising an adorable new rescued kitten. She still has occasional menstrual pain and irritability. It will not surprise me if she breaks out again now and then, and I expect that it will be simple to resolve when she does. The patient is extremely satisfied with the results and is no longer embarrassed by her skin.
References:
- “Adult Acne.” American Academy of Dermatology, www.aad.org/public/diseases/acne/really-acne/adult-acne.
- Bensky, Dan, et al. Chinese Herbal Medicine. Eastland Press, 2015.
- Huang, Fei-li, et al. Cosmetology in Chinese Medicine. People's Medical Publishing House, 2011.
- Huang, Ying, et al. TCM Case Studies. People's Medical Publishing House, 2014.
- Yang, Yifan. Chinese Herbal Medicines: Comparisons and Characteristics. Churchill Livingstone/Elsevier, 2010.
 Juliette Aiyana, L.Ac. is Nationally Board Certified (NCCAOM) and a New York State Licensed Acupuncturist. She is a professor of Chinese medicine, CE seminar teacher, and an author who has been in practice since 2001. Since the pandemic, Ms. Aiyana pivoted her practice from a hybrid in-person herbal and acupuncture practice and online consulting to exclusively providing online herbal and holistic virtual consulting. Ms. Aiyana specializes in the treatment of chronic and stubborn diseases such as dermatology, autoimmune disorders, allergies, digestive disorders, menstrual disorders, menopausal symptoms, chronic fatigue, migraines, anxiety and more. www.julietteaiyana.com, Instagram @julietteaiyananaturalhealth
Juliette Aiyana, L.Ac. is Nationally Board Certified (NCCAOM) and a New York State Licensed Acupuncturist. She is a professor of Chinese medicine, CE seminar teacher, and an author who has been in practice since 2001. Since the pandemic, Ms. Aiyana pivoted her practice from a hybrid in-person herbal and acupuncture practice and online consulting to exclusively providing online herbal and holistic virtual consulting. Ms. Aiyana specializes in the treatment of chronic and stubborn diseases such as dermatology, autoimmune disorders, allergies, digestive disorders, menstrual disorders, menopausal symptoms, chronic fatigue, migraines, anxiety and more. www.julietteaiyana.com, Instagram @julietteaiyananaturalhealth

